How men continually produce sperm—and how that discovery could help treat infertility
The production of sperm—otherwise known as spermatogenesis—generates more than 1,000 sperm per second in normal males. This productivity comes, in part, from a special cell type called the spermatogonial stem cell. The staying power of this stem cell has allowed many celebrities, including Robert DeNiro and Pablo Picasso, to father children after the age of 65.
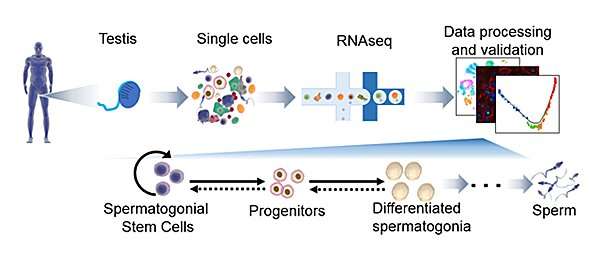
Yet spermatogonial stem cells have not been well studied in humans, and attempts to grow them in the lab for clinical purposes have had limited success. In a study published February 5, 2019 in Cell Reports, researchers at University of California San Diego School of Medicine used a technique called single-cell RNA sequencing to develop a clearer picture of human spermatogonial stem cells and how sperm are formed. They also developed tools to better isolate these stem cells.
This advance, the researchers write, opens the possibility that spermatogonial stem cell transplants could be developed to treat male infertility, an issue that affects more than 100 million men worldwide.
"Single-cell RNA sequencing determines the activity of hundreds of genes in the genomes of single cells," said senior author Miles Wilkinson, Ph.D., professor in the Department of Obstetrics, Gynecology and Reproductive Sciences at UC San Diego School of Medicine. "Because each cell type has a different combination of active genes, this technique allows new cell types to be identified. Applying this approach to the testis, we uncovered many different stages of sperm precursor cells in human testes."
In adult human testes, the researchers identified several cell subtypes that likely include spermatogonial stem cells. They also found cells with the characteristics of spermatogonial stem cells in human newborns.
"Given that spermatogonial stem cells are not necessary for generating sperm until puberty, this finding in newborns raises the possibility that these cells perform as-of-yet unknown functions in infants and young children," Wilkinson said.
Their study also identified many unique molecules—biomarkers—that define spermatogonial stem cells. These biomarkers, which they detected with specific antibodies, allowed the researchers to efficiently capture human spermatogonial stem cells.
Wilkinson's team also identified the genes active in other cells that support spermatogonial stem cells. The finding may help researchers develop protein cocktails that drive spermatogonial stem cell proliferation in the laboratory, and allow them to scale up enough of the cells for clinical applications.
"This was a proof-of-principal for future clinical studies to use spermatogonial stem cell therapy as a means to treat men suffering from infertility, including cancer patients rendered infertile by chemotherapy," said Wilkinson.
More information: Abhishek Sohni et al. The Neonatal and Adult Human Testis Defined at the Single-Cell Level, Cell Reports (2019). DOI: 10.1016/j.celrep.2019.01.045
Journal information: Cell Reports
Provided by University of California - San Diego


















